Tylenol (acetaminophen) is one of the most widely used over-the-counter medications for pain relief and fever reduction.
While it’s generally safe when used correctly, getting the right dosage is crucial for both effectiveness and safety—especially when it comes to children. This is where weight-based dosing comes into play.
Weight-based dosing refers to adjusting the amount of Tylenol given based on an individual’s body weight, which helps ensure that they receive the correct therapeutic dose without risking overdose or underdose.
For children, weight-based dosing is particularly important, as their bodies process medications differently than adults.
Inadequate doses can lead to ineffective treatment, while excessive amounts can cause serious harm, such as liver damage.
In this article, we’ll explore the importance of weight-based dosing for Tylenol, provide clear guidelines for safe administration, and discuss key considerations for both pediatric and adult patients.
General Dosing Guidelines
Tylenol dosing varies based on age, weight, and specific health needs. Understanding the correct dosage is essential for ensuring the medication works effectively while minimizing the risk of toxicity or side effects. For both adults and children, following the recommended dosing guidelines is key to achieving the right therapeutic effect.
Adult Dosing
For most adults, the typical Tylenol dose is 500 mg every 4–6 hours, not to exceed 4,000 mg in a 24-hour period. This dosage can help manage mild to moderate pain or reduce fever. However, it’s important to consider individual factors, such as underlying medical conditions or other medications, which could affect how Tylenol is metabolized. People with liver disease or those who consume alcohol regularly may need to reduce their dosage, as acetaminophen is primarily processed in the liver.
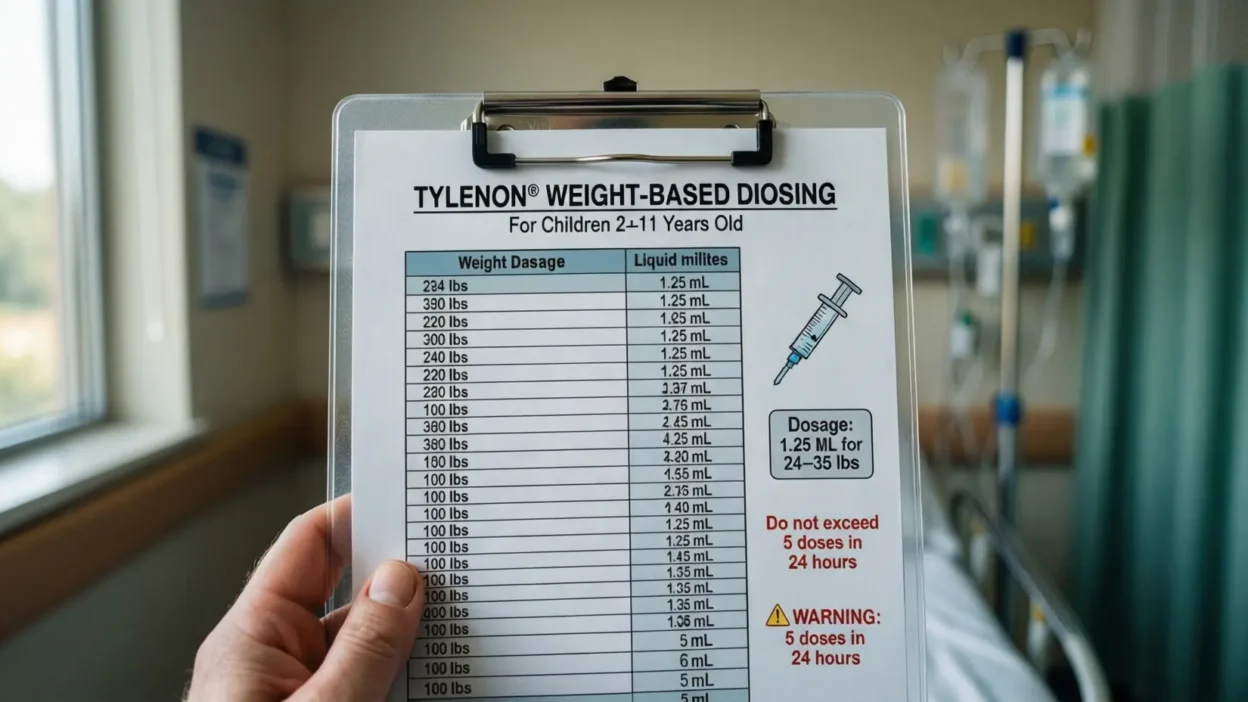
Pediatric Dosing
For children, weight-based dosing is crucial. The standard range for Tylenol in pediatric patients is typically 10-15 mg per kilogram of body weight, per dose. For example, a 20 kg child should receive between 200–300 mg per dose, with a maximum of five doses in a 24-hour period. The dosing frequency depends on the severity of symptoms and the child’s overall health. Infants and young children often receive Tylenol in liquid form to make it easier to measure and administer.
It’s essential to use an accurate dosing tool, such as a syringe or calibrated cup, to ensure the proper amount is given. Miscalculating the dose, especially in young children, can have serious consequences. Always consult a healthcare provider if unsure about the right dosage.
Why Weight-Based Dosing Matters
Weight-based dosing is crucial for ensuring that Tylenol provides effective pain relief or fever reduction without causing harm. The pharmacokinetics of acetaminophen—how the body absorbs, distributes, metabolizes, and excretes the drug—are influenced by body weight, making individualized dosing essential. For both children and adults, using weight-based guidelines ensures that the correct amount of the drug reaches the bloodstream to provide therapeutic benefits while minimizing the risk of overdose.
Pharmacokinetics of Acetaminophen
The way acetaminophen is processed in the body differs based on weight. A child who weighs less will have a smaller volume of distribution and may process the medication more quickly. On the other hand, larger individuals or those with higher body fat percentages may need higher doses to achieve the same effects because the drug distributes differently in a larger body mass. Therefore, weight-based dosing helps tailor the treatment to the specific needs of the individual.
Risks of Incorrect Dosing
Incorrect dosing—whether too much or too little—can lead to serious health risks. Underdosing may result in ineffective pain relief or fever reduction, leaving symptoms untreated. Overdosing, however, is far more dangerous and can lead to acetaminophen toxicity, which can cause liver damage, kidney failure, and in extreme cases, death. Since acetaminophen is metabolized by the liver, exceeding the recommended dose can overwhelm this organ, leading to irreversible damage.
To avoid these risks, it’s essential to follow weight-based dosing instructions carefully, especially for children whose smaller bodies are more sensitive to medication.
Detailed Dosing Calculations
When it comes to administering Tylenol, the correct dosage is crucial for ensuring both safety and effectiveness. For pediatric patients, the recommended dose is typically based on weight, as their smaller bodies process medications differently than adults. To simplify the process, weight-based dosing calculations are essential. Let’s walk through the steps and provide examples to help you calculate the proper dose for children.
Step-by-Step Calculation for Pediatric Dosing
The general formula for weight-based dosing of Tylenol in children is:Dose (mg)=Weight (kg)×Dosing Factor (10-15 mg/kg)\text{Dose (mg)} = \text{Weight (kg)} \times \text{Dosing Factor (10-15 mg/kg)}Dose (mg)=Weight (kg)×Dosing Factor (10-15 mg/kg)
For example, for a child weighing 15 kg (approximately 33 lbs), the calculation would be:Dose=15 kg×10 mg/kg=150 mg(lower end of the dosing range)\text{Dose} = 15 \, \text{kg} \times 10 \, \text{mg/kg} = 150 \, \text{mg} \quad \text{(lower end of the dosing range)}Dose=15kg×10mg/kg=150mg(lower end of the dosing range)
ORDose=15 kg×15 mg/kg=225 mg(higher end of the dosing range)\text{Dose} = 15 \, \text{kg} \times 15 \, \text{mg/kg} = 225 \, \text{mg} \quad \text{(higher end of the dosing range)}Dose=15kg×15mg/kg=225mg(higher end of the dosing range)
So, for this 15 kg child, the correct Tylenol dose would fall between 150 mg and 225 mg per dose.
Adjusting for Age and Special Conditions
While weight is the primary factor, age and health conditions also play a role. For example, younger children or infants may be given smaller doses, even if they fall within the weight range. Special considerations like liver or kidney issues, or obesity, might require dose adjustments.
It’s crucial to consult with a healthcare provider to ensure that the appropriate dose is given based on the child’s weight, age, and medical condition.
Signs of Tylenol Overdose and What to Do
Acetaminophen, while effective when taken correctly, poses significant risks if overdosed. The liver metabolizes Tylenol, and excessive amounts can overwhelm this organ, leading to toxicity. It’s crucial for both parents and adults to recognize the signs of a Tylenol overdose early and take immediate action to prevent serious health complications.
Symptoms of Acetaminophen Overdose
The symptoms of a Tylenol overdose may not appear immediately, making it more dangerous. Within the first few hours, a person might not experience any noticeable signs. However, as time progresses, symptoms can emerge. These include:
- Nausea and Vomiting: These are often the first signs of overdose.
- Abdominal Pain: Pain or discomfort in the upper abdomen, where the liver is located, may indicate liver damage.
- Loss of Appetite: A reduced desire to eat, sometimes accompanied by feelings of fatigue.
- Sweating and Confusion: As the body processes the excess acetaminophen, confusion, dizziness, or even severe lethargy can occur.
- Jaundice: Yellowing of the skin or eyes is a late sign of liver failure.
What to Do if Overdose Is Suspected
If you suspect a Tylenol overdose, seek immediate medical attention. In cases of accidental overdose, calling Poison Control or going to the nearest emergency room is essential. The sooner medical help is received, the better the chances of preventing long-term liver damage.
Doctors may administer an antidote, N-acetylcysteine (NAC), which can help reduce liver damage when given within hours of the overdose. Early intervention is critical to recovery.
Tips for Safe Administration of Tylenol
Ensuring the safe use of Tylenol (acetaminophen) requires careful attention to the correct dosage, timing, and method of administration. This is especially important for parents giving Tylenol to children, as well as for adults managing their own medications. By following these key guidelines, you can minimize the risks associated with Tylenol use and ensure its effectiveness.
1. Use the Right Measurement Tools
When administering Tylenol, especially to children, always use the correct measuring tool provided with the medication. Dosing spoons, syringes, or cups are designed for accuracy and should be preferred over household teaspoons or tablespoons, which can lead to incorrect dosing. Ensure that you read the measurements carefully to avoid underdosing or overdosing.
2. Check the Label and Follow Instructions
Always read the label carefully, especially for liquid forms of Tylenol. The concentration of acetaminophen can vary depending on the product, and this will affect the dosage. For example, infant drops often contain a higher concentration of acetaminophen than liquid formulations for older children. Make sure you’re administering the correct concentration based on your child’s weight and age.
3. Be Mindful of Other Medications
Many over-the-counter and prescription medications contain acetaminophen, so it’s important to check other medications your child or yourself may be taking to avoid exceeding the recommended daily limit. Accidental overdose can occur if multiple sources of acetaminophen are taken together.
4. Set Timely Reminders
Tylenol is typically administered every 4–6 hours. Set reminders on your phone or mark the time on a calendar to avoid giving doses too soon, which can lead to dangerous accumulation in the system.
When to Consult a Healthcare Provider
Although Tylenol is widely regarded as safe when used correctly, there are times when consulting a healthcare provider becomes necessary. Whether it’s for dosing concerns, potential side effects, or interactions with other medications, understanding when to reach out for professional advice is vital for safety.
1. Uncertainty About the Correct Dosage
One of the most common reasons to consult a healthcare provider is uncertainty about the correct Tylenol dosage. If you are unsure whether to follow the recommended guidelines based on weight, age, or other factors (such as liver conditions or other medications), it’s essential to get expert advice. This is especially critical for parents, as dosing errors can have serious consequences for children.
2. Pre-existing Medical Conditions
If you or your child has a pre-existing liver or kidney condition, a history of alcohol use, or any other chronic illness, the way your body processes acetaminophen may be altered. In these cases, dosing may need to be adjusted to avoid strain on the liver. It’s important to inform your healthcare provider of any such conditions before administering Tylenol.
3. Signs of Overdose or Side Effects
If you notice any signs of overdose or side effects, such as persistent nausea, abdominal pain, jaundice (yellowing of the skin or eyes), or confusion, seek immediate medical attention. Early intervention can prevent serious health issues, particularly liver damage. If any unusual symptoms appear after taking Tylenol, contact a healthcare provider right away.
4. Long-Term Use or Frequent Dosing
If Tylenol is being used frequently or for extended periods of time to manage chronic pain or fever, it’s important to consult a healthcare provider to ensure it is still the best treatment option. Long-term use of acetaminophen can increase the risk of liver damage and other complications.
Alternatives to Tylenol (Acetaminophen) for Pain Relief
While Tylenol (acetaminophen) is effective for pain relief and fever reduction, it’s not the only option available. For some individuals, especially those with liver issues or who need longer-term relief, other alternatives may be a safer or more appropriate choice. Understanding these options allows for more informed decisions about pain management, tailored to individual needs.
1. Ibuprofen (Advil, Motrin)
Ibuprofen is a nonsteroidal anti-inflammatory drug (NSAID) that works by reducing inflammation, which makes it effective for treating conditions like muscle aches, arthritis, and headaches, in addition to fever and pain. Unlike Tylenol, ibuprofen works through a different mechanism by inhibiting the production of prostaglandins, chemicals in the body that promote inflammation. However, ibuprofen should be taken with food to avoid gastrointestinal irritation and may not be suitable for people with certain kidney issues or ulcers.
2. Aspirin
Aspirin, another NSAID, is similar to ibuprofen in that it reduces inflammation and alleviates pain. It’s particularly useful for conditions like headaches, toothaches, and minor aches and pains. However, aspirin is generally not recommended for children under 18 due to the risk of Reye’s syndrome, a rare but serious condition. Additionally, aspirin can cause gastrointestinal irritation and bleeding in some individuals, particularly those with a history of ulcers.
3. Natural Alternatives
For those seeking natural remedies, options like turmeric (curcumin), ginger, and capsaicin have shown potential in reducing pain and inflammation. These alternatives may not be as fast-acting as pharmaceutical options, but they may be worth considering for chronic, low-level pain or inflammation.
4. Topical Analgesics
Topical creams or gels containing menthol, camphor, or lidocaine can provide localized pain relief for conditions like muscle strains, joint pain, or arthritis. These treatments work by numbing the area or providing a cooling sensation that distracts from pain.
How to Prevent Tylenol Overdose in Children
While Tylenol is a safe and effective medication for treating mild to moderate pain and fever in children, it’s crucial to administer it correctly to prevent overdose. Children’s smaller bodies require precise dosing, and any mistake can lead to serious consequences. Here are key strategies to ensure the safe use of Tylenol in children:
1. Always Use the Correct Dosing Tool
For accurate dosing, always use the measuring tool that comes with the medication, such as a syringe or calibrated dosing cup. Avoid using household teaspoons or tablespoons, as they can be inaccurate and lead to the wrong amount of medication being given. If your child is prescribed a liquid form of Tylenol, be sure to check the concentration to ensure you’re administering the correct dose based on your child’s weight and age.
2. Follow Weight-Based Dosing Guidelines
Weight-based dosing is especially important for children under 12. The dose of Tylenol for children is usually 10-15 mg per kilogram of body weight per dose, with a maximum of five doses in 24 hours. Before giving any dose, calculate your child’s weight-based dose using a calculator or consult the packaging instructions. If you’re unsure, consult a healthcare provider to verify the correct dose.
3. Keep Track of Doses
It’s easy to forget when the last dose was administered, so keep a log of each dose given. This will help you avoid giving too many doses within a 24-hour period, which could lead to overdose. Setting reminders on your phone or using a calendar can also help you stay on track.
4. Store Medication Safely
To prevent accidental ingestion, always store Tylenol out of reach of children. Store it in a high, locked cabinet, and ensure the cap is tightly secured. Children are often curious, and even a small extra dose of Tylenol can be dangerous.
The Role of Tylenol in Managing Fever
Fever is a common symptom of various illnesses, from mild infections to more serious conditions. While it is the body’s natural response to fighting off infections, fever can cause discomfort and be concerning, especially in children. Tylenol (acetaminophen) plays an important role in managing fever by helping to lower the body’s temperature and alleviate discomfort, making the person feel better while the immune system works to address the underlying cause.
How Tylenol Works to Reduce Fever
Tylenol works by targeting the hypothalamus, the part of the brain responsible for regulating body temperature. When the body detects an infection, the hypothalamus raises the body’s temperature as a defense mechanism. Acetaminophen helps to reset this thermostat to a lower level, effectively reducing fever and promoting a more comfortable state. While Tylenol is effective in lowering fever, it doesn’t cure the underlying infection; it simply provides relief from the discomfort associated with fever.
When to Use Tylenol for Fever Management
Tylenol is typically recommended for managing mild to moderate fever in children and adults, especially when the fever is causing discomfort. A fever in itself is not necessarily dangerous unless it reaches high temperatures (above 104°F or 40°C), but high fever can be distressing, particularly in young children. In general, Tylenol should be used when the fever is causing significant discomfort or is above 100.4°F (38°C), but it’s important not to rely on it as the sole treatment.
When Not to Use Tylenol
Tylenol is generally not recommended for use in treating fevers caused by specific conditions, such as certain viral infections like chickenpox or influenza, where fever is part of the body’s natural defense. In some cases, using fever-reducing medications like Tylenol could mask important symptoms or delay a diagnosis. It’s always important to consult with a healthcare provider if a fever persists or if it’s accompanied by other worrying symptoms.
Long-Term Use of Tylenol: Risks and Considerations
While Tylenol (acetaminophen) is considered safe for short-term use, particularly for managing pain and fever, prolonged or frequent use can lead to significant risks. These risks are particularly concerning for individuals who rely on Tylenol for chronic pain relief or who take it on a daily basis. Understanding these risks and taking steps to minimize them is essential for ensuring long-term health.
1. Liver Damage
The most significant risk associated with long-term Tylenol use is liver damage. Tylenol is metabolized by the liver, and taking too much can overwhelm this organ, leading to hepatotoxicity (liver damage). Chronic use, especially at high doses or combined with alcohol, can result in serious liver conditions, including acute liver failure. Individuals who already have liver disease or a history of alcohol abuse should be particularly cautious about using acetaminophen regularly.
2. Kidney Damage
While liver damage is the primary concern, excessive use of Tylenol can also affect kidney function. Some studies suggest that long-term acetaminophen use can increase the risk of kidney disease, especially in individuals who take the drug in combination with other substances that strain the kidneys, such as nonsteroidal anti-inflammatory drugs (NSAIDs).
3. Tolerance and Overuse
Chronic use of Tylenol for managing persistent pain may lead to tolerance, where higher doses are needed to achieve the same effect. This can increase the risk of overdose, especially if other medications containing acetaminophen are also being used simultaneously. Over time, individuals may inadvertently consume toxic levels of acetaminophen.
4. Safe Use Recommendations for Chronic Pain
For those who need ongoing pain management, it’s essential to explore alternatives to Tylenol, such as NSAIDs (like ibuprofen) or other pain management strategies that don’t rely on acetaminophen. Always discuss your pain management plan with a healthcare provider to ensure you’re using the safest approach for your specific situation.
Understanding the Tylenol Dosing Schedule
Properly managing the dosing schedule for Tylenol (acetaminophen) is crucial to ensure its effectiveness and safety. Tylenol is often used to alleviate mild to moderate pain and reduce fever, but taking it incorrectly can lead to serious health risks, including overdose. Whether for children or adults, understanding how often to administer Tylenol and following the recommended guidelines is essential to avoid complications.
1. Recommended Dosing Intervals
For most people, the recommended dosing interval for Tylenol is every 4 to 6 hours. This allows enough time for the medication to take effect and for the body to process it without reaching toxic levels. Adults should not take more than 4,000 mg of acetaminophen per day, and children’s dosages are based on weight and age.
2. Avoiding Overdose: The Importance of Timing
Overdosing on Tylenol can cause serious liver damage, as the liver becomes overwhelmed when processing too much acetaminophen in a short period of time. To prevent this, make sure that doses are spaced appropriately. It’s easy to forget when the last dose was taken, so it’s helpful to keep track, either on paper or with a smartphone reminder, especially if you’re administering Tylenol to a child.
3. The Role of Hepatic Metabolism
The liver metabolizes Tylenol, and excessive or frequent doses can cause hepatic toxicity. This is why sticking to the recommended dosing schedule is especially important for individuals with pre-existing liver conditions or those who take multiple medications that may strain the liver.
4. Special Considerations for Different Age Groups
For infants and children, dosing should always be based on weight, as children metabolize medications differently than adults. The packaging of children’s Tylenol often includes specific weight-based guidelines to help ensure the correct dosage. Always consult the dosing instructions on the package and consider contacting a healthcare provider if you have any doubts about the correct amount.
Tylenol and Alcohol: Understanding the Risks
Combining Tylenol (acetaminophen) with alcohol poses significant risks to your health, particularly to the liver. While both Tylenol and alcohol are commonly used, their effects on the liver can be dangerous when combined, leading to serious health complications. Understanding how these substances interact and the risks involved is crucial for preventing liver damage and other health issues.
1. The Impact on the Liver
Tylenol is primarily metabolized in the liver, and excessive use can put strain on this organ. Alcohol, too, is processed by the liver, and chronic alcohol consumption can lead to liver damage. When you combine alcohol with Tylenol, the liver is forced to process both substances at once, increasing the risk of hepatotoxicity (liver toxicity). Even moderate drinking while using Tylenol can heighten the risk of liver damage over time.
2. Increased Risk of Liver Failure
The combination of Tylenol and alcohol can accelerate liver damage, potentially leading to acute liver failure, a life-threatening condition. This is especially true for individuals who consume alcohol regularly or in large quantities. Even the standard daily dose of acetaminophen (4,000 mg) can cause liver problems when taken alongside alcohol, particularly in individuals who drink heavily or have a history of liver disease.
3. Symptoms of Liver Damage
Symptoms of liver damage from the combination of alcohol and Tylenol may include nausea, vomiting, loss of appetite, abdominal pain, jaundice (yellowing of the skin or eyes), and confusion. If you experience any of these symptoms, seek medical attention immediately, as early intervention can prevent serious complications.
4. Guidelines for Safe Use
If you consume alcohol regularly, it’s advisable to avoid using Tylenol altogether or limit its use to occasional instances when you need pain or fever relief. For individuals who drink heavily or have a history of liver disease, consult a healthcare provider before using Tylenol to understand the safest alternatives. As a general rule, always avoid drinking alcohol while taking any medication that can affect the liver, including acetaminophen.
Signs of Tylenol Overdose and When to Seek Medical Help
Tylenol (acetaminophen) is generally safe when used correctly, but taking too much can lead to overdose, a potentially life-threatening condition. Overdose can occur accidentally, especially if someone takes multiple doses in a short period, consumes other medications containing acetaminophen, or miscalculates the dose. Recognizing the early signs of overdose and knowing when to seek medical help is crucial for preventing severe liver damage and other complications.
1. Early Symptoms of Tylenol Overdose
In the first few hours after taking an overdose, you may not notice any symptoms, which is why Tylenol overdoses can be deceptive. However, as the acetaminophen is metabolized by the liver, you might begin to experience the following symptoms:
- Nausea and vomiting
- Loss of appetite
- Abdominal pain or tenderness, particularly in the upper right side
- Fatigue or weakness
- Sweating
At this stage, it’s important to seek medical attention, as the liver may still be able to recover with prompt treatment.
2. Severe Symptoms of Tylenol Overdose
If the overdose is not treated in time, the symptoms can worsen, leading to severe liver damage. Later symptoms may include:
- Jaundice (yellowing of the skin or eyes)
- Dark urine
- Clay-colored stools
- Confusion or disorientation
- Bleeding or easy bruising
These signs indicate liver failure and require immediate medical attention. Without treatment, the damage can become irreversible, potentially leading to death.
3. What to Do in Case of an Overdose
If you suspect an overdose, call a poison control center or seek emergency medical help immediately. Time is critical in treating Tylenol overdose, and early intervention can significantly reduce the risk of permanent damage. In some cases, an antidote known as N-acetylcysteine (NAC) can be administered to prevent liver damage if given within hours of the overdose.
Alternatives to Tylenol for Pain and Fever Management
While Tylenol (acetaminophen) is widely used for pain and fever relief, there are various alternatives available for those who need or prefer to avoid acetaminophen, whether due to health concerns or personal preference. Choosing the right medication depends on the underlying condition, age, and overall health of the individual. Below are some commonly recommended alternatives to Tylenol for managing pain and fever.
1. Ibuprofen (Advil, Motrin)
Ibuprofen is a nonsteroidal anti-inflammatory drug (NSAID) that works by reducing inflammation, pain, and fever. It’s effective for managing conditions such as headaches, muscle aches, arthritis, and fever. Unlike Tylenol, which is metabolized in the liver, ibuprofen is processed by the kidneys, so it may be a better choice for individuals with liver concerns. However, it’s important to be cautious with ibuprofen in individuals with kidney disease or gastrointestinal issues, as it can cause irritation or ulcers in the stomach lining.
2. Aspirin
Aspirin, another NSAID, is often used for pain relief, inflammation reduction, and fever management. It is commonly used for conditions like headaches, menstrual pain, and minor arthritis. Like ibuprofen, aspirin should be avoided in children under 18 for fever management due to the risk of Reye’s syndrome, a rare but serious condition that can cause liver and brain damage.
3. Naproxen (Aleve)
Naproxen is another NSAID that works similarly to ibuprofen but lasts longer. It is typically taken every 8 to 12 hours, making it a good option for managing chronic pain or inflammation. As with other NSAIDs, it should be used cautiously in individuals with a history of gastrointestinal issues or kidney disease.
4. Non-Pharmacological Alternatives
For those seeking non-medication options, several non-pharmacological treatments can help manage pain and fever:
- Cold compresses for reducing fever
- Hydration to prevent dehydration from fever
- Rest and relaxation to aid recovery
- Massage and physical therapy for muscle pain
These alternatives may not be as immediate as medications, but they can be effective in combination with other treatments for mild conditions.
Precautions and Safety Tips for Using Tylenol
While Tylenol (acetaminophen) is generally considered safe for most individuals when used correctly, there are several important precautions and safety tips to keep in mind to avoid potential risks, including overdose and liver damage. Following proper guidelines and being aware of certain health conditions can ensure that Tylenol remains a safe and effective option for pain and fever relief.
1. Know the Correct Dosage
One of the most important safety tips is to always follow the recommended dosage instructions on the packaging or as directed by your healthcare provider. For adults, the maximum daily dose is generally 4,000 mg, which is typically broken down into doses of 500 to 1,000 mg every 4 to 6 hours. It’s important not to exceed this amount, as doing so can overwhelm the liver, leading to severe damage. For children, dosing should be based on age and weight, and it’s essential to use the correct form (liquid, chewable, etc.) and dosing tool provided.
2. Avoid Combining with Other Acetaminophen Products
Many over-the-counter and prescription medications contain acetaminophen, so it’s easy to accidentally take more than the recommended dose. Common medications like cold, flu, and pain relief products may contain acetaminophen, so always check the labels before using multiple products. Combining acetaminophen-containing medications can significantly increase the risk of overdose, even if each individual product is taken within the recommended dose.
3. Use Caution with Liver Disease and Alcohol Use
Individuals with pre-existing liver disease or a history of heavy alcohol consumption should consult with a healthcare provider before using Tylenol. Both conditions increase the risk of liver damage, especially when combined with acetaminophen. If you regularly consume alcohol, it’s best to limit Tylenol use or avoid it altogether, as the combination can place significant strain on the liver.
4. Monitor for Side Effects
While Tylenol is generally well-tolerated, some people may experience allergic reactions or side effects, such as skin rash, swelling, or difficulty breathing. If any of these symptoms occur, seek medical help immediately. Additionally, if you experience symptoms of liver damage (such as jaundice, dark urine, or severe abdominal pain), stop using Tylenol and seek urgent medical care.
Tylenol for Children: Safe Use and Dosage Guidelines
Tylenol (acetaminophen) is commonly used to treat fever and mild to moderate pain in children, but it is important to follow specific guidelines to ensure its safe and effective use. Since children’s bodies process medications differently from adults, careful attention to dosage, frequency, and age-appropriate formulations is crucial to avoid accidental overdose or side effects.
1. Dosage Based on Weight and Age
For children, the correct dose of Tylenol is typically determined by weight, not age. This is because children grow at different rates, and weight is a more accurate measure of their ability to metabolize the medication. The dosing instructions on the Tylenol packaging or the guidance from a pediatrician should be followed precisely. The general recommendation is usually 10-15 mg per kilogram of body weight every 4 to 6 hours, but the total daily dose should not exceed the maximum recommended amount, which is 4,000 mg per day for children.
2. Choosing the Right Formulation
Tylenol for children comes in several formulations, including liquids, chewable tablets, and suppositories. Liquid formulations are often easier for younger children to take, but it’s crucial to use the correct measuring tool (e.g., dosing cup or syringe) to ensure accuracy. Chewable tablets or tablets are suitable for older children who can safely swallow them, and suppositories may be used if a child is unable to take medicine orally due to vomiting or other reasons.
3. Avoiding Overdose and Harmful Interactions
The risk of Tylenol overdose is particularly high in children, so it is essential to avoid combining Tylenol with other medications that also contain acetaminophen. Be sure to check the labels of all medications, including those for cold, flu, or cough, to ensure acetaminophen isn’t included. Overdose symptoms in children can include nausea, vomiting, loss of appetite, and abdominal pain. If any of these symptoms occur, contact a healthcare professional immediately.
4. When to Consult a Doctor
Before giving Tylenol to children, especially if they are younger than 3 months old, it’s best to consult a doctor for dosing recommendations. For children with chronic health conditions or who are taking other medications, it’s particularly important to discuss the safety of acetaminophen with a healthcare provider.
Understanding the Role of Tylenol in Chronic Pain Management
Chronic pain is a persistent condition that can significantly impact daily life, making effective management essential for improving quality of life. While Tylenol (acetaminophen) is often used to treat acute pain, its role in managing chronic pain is more nuanced. Understanding when and how to use Tylenol for long-term pain management is important for minimizing potential risks, such as liver damage, while maximizing its effectiveness.
1. Effectiveness of Tylenol for Chronic Pain
Tylenol is a mild to moderate pain reliever that is often used for conditions like arthritis, back pain, and muscle pain. Unlike nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen, Tylenol does not have anti-inflammatory properties, which means it may be less effective for conditions that involve inflammation, such as osteoarthritis. However, for pain that does not involve significant inflammation, Tylenol can be an effective choice for managing mild to moderate chronic pain.
2. Benefits of Tylenol for Chronic Pain
One of the advantages of using Tylenol for chronic pain management is that it is generally well-tolerated and has fewer side effects than NSAIDs, especially for individuals with a history of gastrointestinal issues or kidney problems. It is also a safer option for people with liver concerns, as long as the dosage is carefully monitored and not exceeded.
3. Risks and Considerations
While Tylenol can be effective for long-term pain management, it is important to use it cautiously to avoid overdose and liver damage. The maximum daily dose for adults is typically 4,000 mg, but for those managing chronic pain over an extended period, even this amount can be risky. Long-term use of Tylenol should be monitored by a healthcare provider to ensure that the liver is not being compromised, and the individual is not at risk for potential adverse effects.
4. Combining Tylenol with Other Pain Management Strategies
In many cases, Tylenol is used as part of a multifaceted approach to managing chronic pain. This may include physical therapy, lifestyle changes, complementary therapies (such as acupuncture or massage), and the use of stronger prescription pain medications when necessary. Consulting with a doctor is essential to creating a comprehensive pain management plan that minimizes risks and addresses the root causes of pain.
Tylenol Use During Pregnancy
Pregnancy brings additional considerations when it comes to medication use. Tylenol is considered safe for short-term use during pregnancy, particularly for treating mild to moderate pain or fever. It’s also important to avoid excessive use, as prolonged or high doses of acetaminophen during pregnancy may be linked to certain risks, such as potential developmental issues in the baby. As with any medication, Tylenol should only be used during pregnancy when the benefits outweigh the potential risks.
Tylenol Use in Individuals with Pre-existing Conditions
People with pre-existing liver disease, kidney problems, or a history of alcohol abuse need to be particularly cautious when using Tylenol. In these cases, acetaminophen may place additional stress on the liver, increasing the risk of liver damage or failure. For individuals with renal (kidney) issues, Tylenol may be safer than NSAIDs like ibuprofen, but it should still be used with care, particularly in high doses or long-term use. Always consult with a healthcare provider before using Tylenol in the presence of any of these conditions.
The Impact of Tylenol on Liver Health: What You Need to Know
Tylenol (acetaminophen) is a widely used pain reliever and fever reducer, but its potential impact on liver health is one of the most important safety concerns associated with its use. Although Tylenol is generally considered safe when taken as directed, overuse or misuse can lead to severe liver damage, a condition that can be life-threatening. Understanding how Tylenol affects the liver, recognizing signs of liver damage, and taking precautions can help minimize the risks associated with this common medication.
1. How Tylenol Affects the Liver
When Tylenol is metabolized in the body, most of it is processed by the liver without causing harm. However, a small portion is converted into a highly toxic byproduct called NAPQI (N-acetyl-p-benzoquinone imine). Under normal circumstances, the liver neutralizes NAPQI with the help of glutathione, an antioxidant. However, when Tylenol is taken in high doses or over an extended period, glutathione stores can become depleted, allowing NAPQI to accumulate and cause liver cell damage. This process can lead to acute liver failure if not promptly addressed.
2. Signs of Liver Damage
The signs of liver toxicity can be subtle at first, making it essential to be vigilant when using Tylenol for prolonged periods. Symptoms of liver damage include:
- Jaundice (yellowing of the skin or eyes)
- Dark urine
- Abdominal pain or discomfort (particularly in the upper right side of the abdomen)
- Nausea and vomiting
- Loss of appetite
If any of these symptoms occur after using Tylenol, it is crucial to stop using the medication immediately and seek medical attention.
3. Preventing Liver Damage from Tylenol
To reduce the risk of liver damage while using Tylenol, it is essential to follow the recommended dosage and avoid exceeding the daily limit of 4,000 mg for adults. If you are taking other medications that contain acetaminophen, make sure to check labels carefully to avoid accidental overdose. People with pre-existing liver conditions or those who consume alcohol regularly should consult their healthcare provider before using Tylenol to assess whether it’s safe for them.
Overdose and What to Do in Case of a Tylenol Overdose
While Tylenol (acetaminophen) is safe when used correctly, overdose is a significant risk, particularly because its harmful effects can be delayed and may not be immediately obvious. A Tylenol overdose can lead to liver failure, a potentially life-threatening condition that requires urgent medical intervention. Understanding the signs of an overdose and knowing what actions to take can make a critical difference in preventing serious health complications.
1. Symptoms of Tylenol Overdose
The symptoms of a Tylenol overdose often develop in stages, which can make it difficult to recognize in the early hours. Typically, symptoms will start appearing within 4 to 24 hours after ingesting a harmful dose. Early symptoms include:
- Nausea and vomiting
- Loss of appetite
- Abdominal pain (especially in the upper right side of the abdomen)
- Sweating and fatigue
If the overdose is not treated in the early stages, it can progress to more severe symptoms, including:
- Jaundice (yellowing of the skin or eyes)
- Confusion or altered mental state
- Low blood pressure
- Severe bleeding or bruising
- Severe abdominal swelling
If you or someone you know experiences these symptoms after taking Tylenol, it’s critical to seek immediate medical attention, even if the symptoms seem mild at first.
2. What to Do in Case of a Tylenol Overdose
If you suspect a Tylenol overdose, the first step is to call emergency services or poison control immediately. Time is of the essence in treating an overdose. A healthcare provider may administer an antidote called N-acetylcysteine (NAC), which can help neutralize the toxic effects of acetaminophen if given within a specific time window (usually within 8 hours of ingestion).
In the emergency room, the medical team will assess the severity of the overdose and may perform tests to measure acetaminophen levels in the blood. The earlier treatment begins, the more likely it is to prevent irreversible liver damage.
3. Prevention of Overdose
To prevent Tylenol overdose, it’s crucial to never exceed the recommended dose and avoid taking multiple medications containing acetaminophen. Always use the correct measuring devices, and if you’re unsure about the proper dosage, consult a healthcare professional. For individuals with liver disease or other pre-existing health conditions, Tylenol should only be used under strict medical supervision.
Frequently Asked Questions (FAQ) about Tylenol
Tylenol (acetaminophen) is a common pain reliever used by millions of people worldwide. However, many have questions about its use, safety, and effectiveness. Below, we address some of the most frequently asked questions to help you better understand how to use Tylenol responsibly.
1. Can I take Tylenol with other medications?
Tylenol is commonly combined with other medications in over-the-counter products, such as cold and flu medications. However, it’s important to check the labels of any other medicines you’re taking to ensure they don’t contain acetaminophen, as this can lead to an overdose. It’s also essential to consult your doctor if you’re on prescription medications, especially those that affect the liver, kidneys, or digestive system.
2. Is Tylenol safe for long-term use?
Tylenol is generally safe when used for short periods to relieve pain or fever. However, long-term use can increase the risk of liver damage, especially if the recommended dosage is exceeded. For those who require ongoing pain relief, it’s essential to consult a healthcare provider to discuss alternative pain management options and monitor liver function.
3. Can I take Tylenol if I have a history of liver disease?
If you have a history of liver disease, you should avoid Tylenol unless directed by a healthcare provider. Acetaminophen is processed by the liver, and overuse can worsen liver conditions. Your doctor may recommend alternative medications or adjust the dosage to reduce the risk of harm.
4. What should I do if I accidentally take too much Tylenol?
If you suspect that you’ve taken an overdose of Tylenol, it is critical to seek medical help immediately. Symptoms of overdose may not appear right away, but early intervention is key. In an emergency, healthcare professionals may administer N-acetylcysteine (NAC), a medication that helps prevent liver damage.
5. Can Tylenol be taken for headaches?
Yes, Tylenol is effective for treating mild to moderate headaches, including tension headaches. It’s important not to exceed the recommended dosage and to avoid using Tylenol too frequently, as overuse can lead to medication-overuse headaches (rebound headaches).
Conclusion:
Tylenol (acetaminophen) remains one of the most widely used over-the-counter medications for pain relief and fever reduction.
Its efficacy in treating mild to moderate pain and its relatively low risk of side effects when used appropriately make it a go-to solution for many.
However, as with any medication, it’s essential to use Tylenol responsibly to avoid adverse effects, particularly liver damage, which can occur with overuse or high doses.
To safely use Tylenol, it’s important to:
- Follow the recommended dosage instructions carefully and never exceed the daily limit.
- Consult a healthcare provider if you have underlying health conditions, are pregnant, or are taking other medications.
- Be mindful of the risk of overdose, and seek immediate medical attention if you suspect you’ve taken too much.
For individuals with chronic pain or specific health concerns, Tylenol may be a suitable part of a comprehensive pain management plan, but it’s always best to consult a doctor to explore the most appropriate treatment options and avoid unnecessary risks.
Tylenol can be a safe and effective pain reliever when used in moderation, but proper understanding and awareness of its potential risks are essential for long-term health and well-being.

Margaret Johnson was an American blues and early jazz vocalist and pianist active during the 1920s. She began her recording career in the early part of that decade, performing in vaudeville and jazz ensembles, and is best remembered for her work in blues music.